Prevent Blindness has declared February AMD Awareness month[1]. Age-related macular degeneration(AMD) is the most common cause of severe loss of eyesight among people 50 and older.
AMD affects the central vision, and with it, the ability to see fine details. With AMD, the macula, a part of the retina in damaged. In its early stages, AMD may have no signs or symptoms, so people may not suspect they have it. In advanced stages, people lose their ability to drive, to see faces, and to read smaller print. AMD by itself does not lead to complete blindness, with no ability to see. However, the loss of central vision in AMD can severely interfere with simple everyday activities.
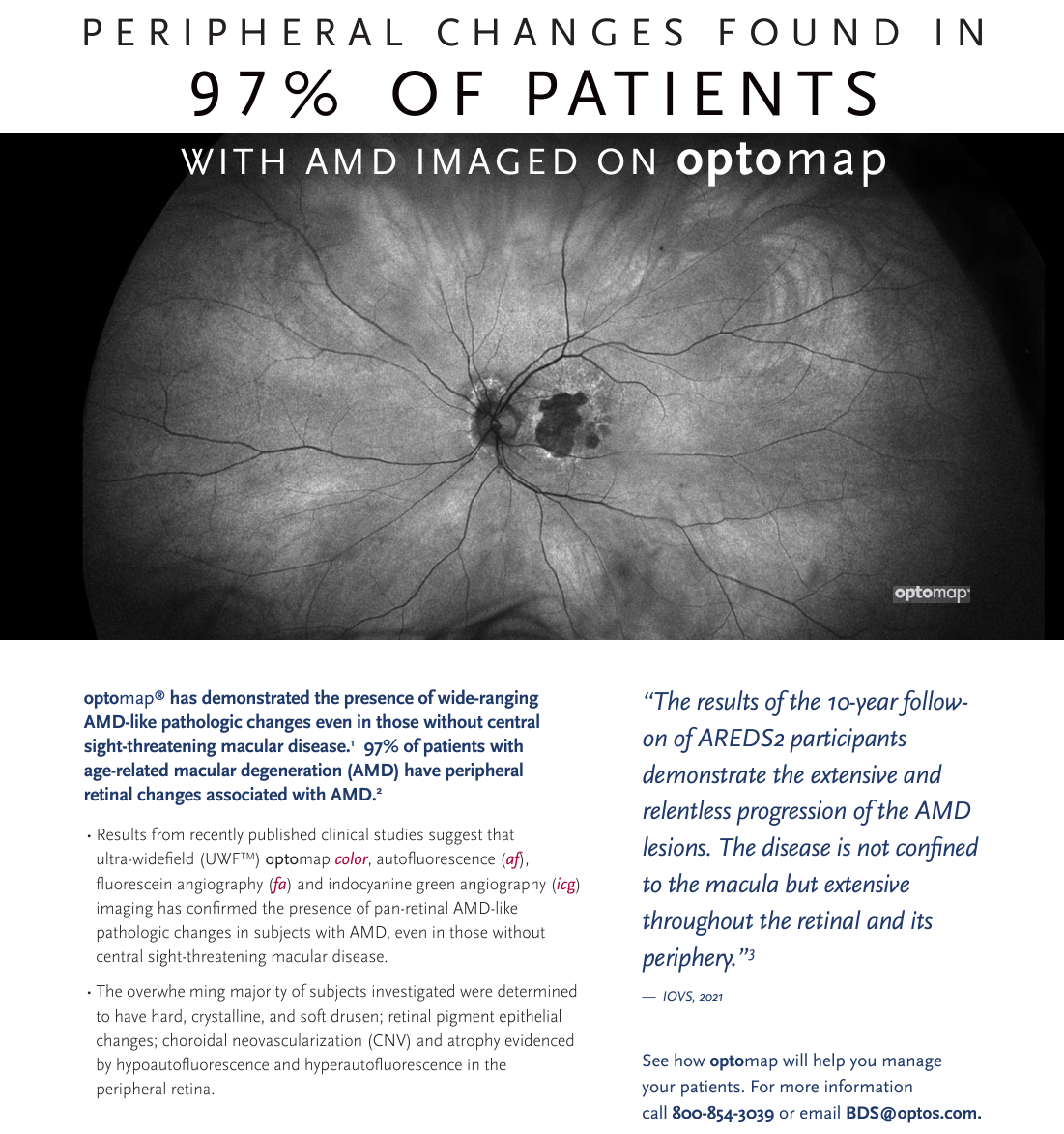
Earlier detection and treatment of AMD can prompt steps to be taken to help reduce vision loss and slow the advance of the disease. Data suggests that the retinal periphery can exhibit some important morphological changes, such as peripheral drusen and reticular pigmentary changes, which are frequently connected with the wet form of AMD. [2]
Typically, disease progression has been documented using fundus cameras that image only about 45-50% percent of the retina. By using ultra-widefield (UWF) for AMD evaluation, over 80% of the retina is now analyzed to record peripheral fluorescein angiographic changes in AMD patients.[3] A wider perspective is also available using both green and blue autofluorescence as well as indocyanine green angiography (icg).
The 12-year follow-up of a study known as the Reykjavik Eye Study evaluated subjects with optomap color and autofluorescence (af) imaging and found that 67% of subjects in the study had peripheral AMD-like changes. Additionally, a subsequent study, knowns as the OPERA (Optos Peripheral RetinA) study found that peripheral retinal changes were more prevalent in eyes with AMD than in those without. Drusen and reticular changes were evident in 97% of the eyes with AMD in both the mid and far periphery.
These studies go to show that AMD may be more than a “macular” condition but one that involves the entire retina. Other research also shows that optomap icg captured significant peripheral changes in 80% of AMD patients4. Additionally, these studies contribute to the benefits of ultra-widefield imaging in the diagnosis and management of AMD.
Longitudinal studies of peripheral changes in AMD and their impact on visual function are underway to further understand the disease, results of the 10 year follow up to the OPERA study will be presented at ARVO 2024.
Recent work presented at Euretina 2023, measurements of GA lesions on UWF FAF images appear to be repeatable and consistent with other imaging modalities.
For more information regarding these studies, or to learn more how ultra-widefield optomap imaging can assist eyecare professionals to find and document AMD earlier and potentially change the course of the disease, contact us today.
[1] https://preventblindness.org/2024-amd-low-vision-month/
[2] Writing Committee for the OPTOS PEripheral RetinA (OPERA) study (Ancillary Study of Age-Related Eye Disease Study 2); Domalpally A, Clemons TE, Danis RP, Sadda SR, Cukras CA, Toth CA, Friberg TR, Chew EY. Peripheral Retinal Changes Associated with Age-Related Macular Degeneration in the Age-Related Eye Disease Study 2: Age-Related Eye Disease Study 2 Report Number 12 by the Age-Related Eye Disease Study 2 Optos PEripheral RetinA (OPERA) Study Research Group. Ophthalmology. 2017 Apr;124(4):479-487. doi: 10.1016/j.ophtha.2016.12.004. Epub 2017 Jan 12. PMID: 28089680.
[3] Kumar V, Surve A, Kumawat D, Takkar B, Azad S, Chawla R, Shroff D, Arora A, Singh R, Venkatesh P. Ultra-wide field retinal imaging: A wider clinical perspective. Indian J Ophthalmol. 2021 Apr;69(4):824-835. doi: 10.4103/ijo.IJO_1403_20. PMID: 33727441; PMCID: PMC8012972.
4 Klufas Et Al. Feasibility and Clinical Utility of Ultra-Widefield Indocyanine Green Angiography. Retina 0:1–13, 2014
5 Sadda. Emerging Treatments and 1st Line Diagnostics for Geographic Atrophy. Euretina. 2023