For eyecare professionals, the comprehensive eye exam is tantamount to patient care. With an investment in multi-modality optomap ultra-widefield (UWF™) retinal imaging the ability to detect pathology, which may be missed with widefield or traditional fundus photography, is a game changer.
optomap UWF retinal imaging is performed by a specially designed scanning laser ophthalmoscope (SLO) that generates high-resolution digital images of 200 degrees (or 82 percent) of the retina, in a single capture. optomap af images are captured using a green wavelength (532nm) to visualize the function of the RPE.
What is Fundus Autofluorescence (FAF)?
FAF is an imaging modality used to provide information on the health and function of the retinal pigment epithelium (RPE). Over time, the retinal photoreceptors naturally age and produce a metabolic waste known as lipofuscin. Lipofuscin is the fatty substance found in the RPE.
Excessive amounts of lipofuscin can be caused by the aging retina, certain retinal diseases and/or the progression of diseases.[1] It has been thought that excessive levels of lipofuscin could affect essential RPE functions that contribute to the progression of age-related macular degeneration (AMD). [2]
These findings have also been shown to have diagnostic value and help to predict which eyes are at greater risk of progression to advanced disease.[3] Typically, FAF imaging has clinical applications in AMD, Geographic Atrophy, central serous retinopathy, choroidal tumors and nevi, inflammatory diseases, inherited disease, optic nerve head drusen, pattern dystrophies, retinal toxicity, and retinal detachments.
optomap af in Practice
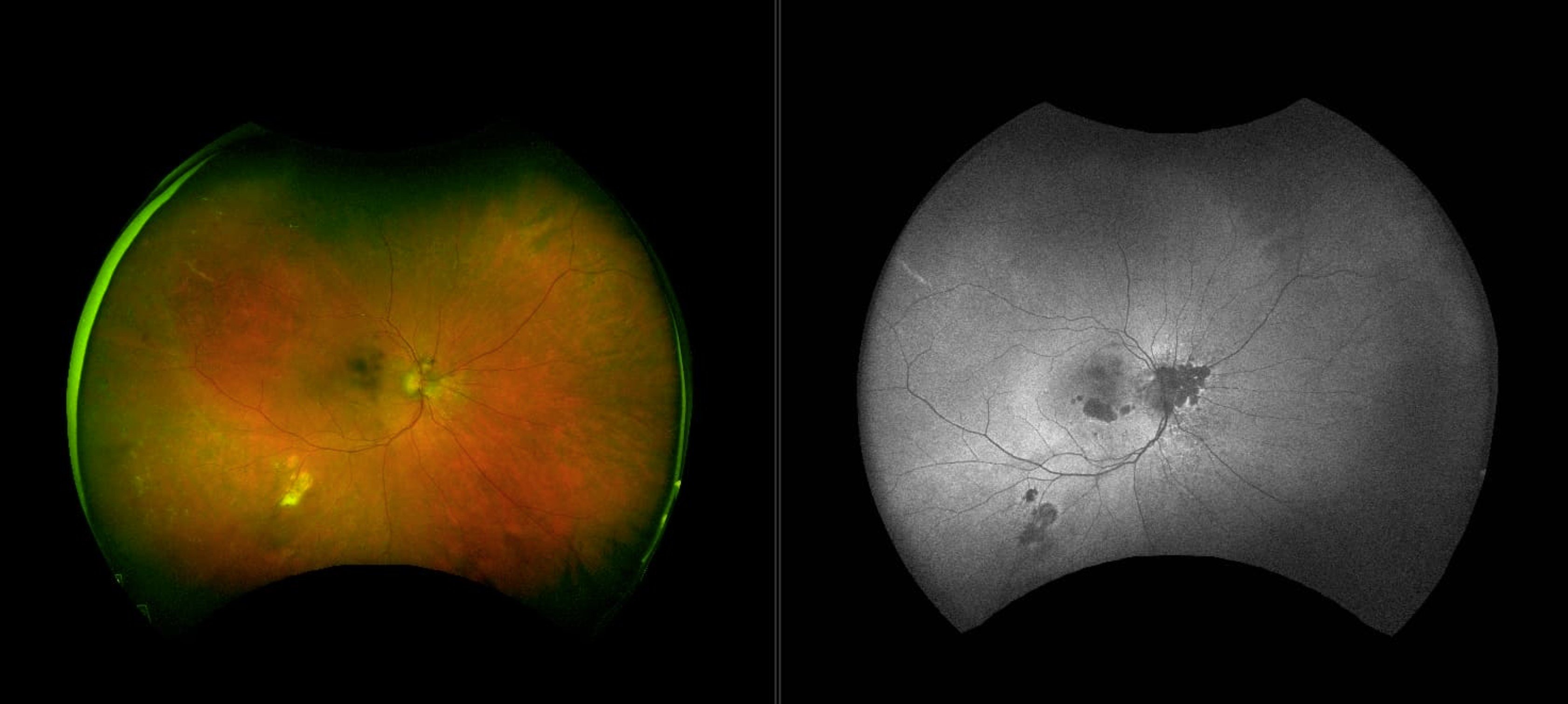
Autofluorescence imaging is a non-invasive study of the fluorescent properties of lipofuscin in the RPE and provides clinical information not available using conventional imaging techniques. optomap af allows for visualization of the metabolic changes at the level of the RPE and helps to identify areas that may be at high risk.
The clinical utility of optomap af is apparent. Studies demonstrating the high prevalence of peripheral autofluorescence changes in AMD, uveitis, retinal dystrophies, and central serous chorioretinopathy (CSCR), further support its relevance in clinical settings. In one study, more than 70% of eyes with AMD have peripheral abnormalities detectable on optomap and optomap af images. Additionally, using optomap af, 57% of eyes with CSCR had peripheral autofluorescence changes undetectable by clinical examination and 49% of eyes had gravitational tracks or gutters signaling past or present fluid movement from the macula to the inferior periphery.
Interpreting optomap af images
Key indicators when interpreting optomap af images:
· The normal RPE yields a slightly granular grey FAF glow in contrast to the optic disc and retinal blood vessels, which appear black.
· Hyperautofluorescence: identifies stressed cells that result in a bright white signal.
· Hypoautofluorescence: dead cells give off no signal which appear dark grey or black.
· optomap af reveals abnormalities that cannot be viewed with other imaging modalities.
Please visit our comprehensive resource page dedicated to optomap af resources