It is estimated that in the United States, choroidal nevi can be found in 4.6 to 7.9 percent of Caucasian individuals1 and that one in approximately 8,000 of these nevi transform into melanoma2. It is this rare ability that makes these lesions clinically significant.
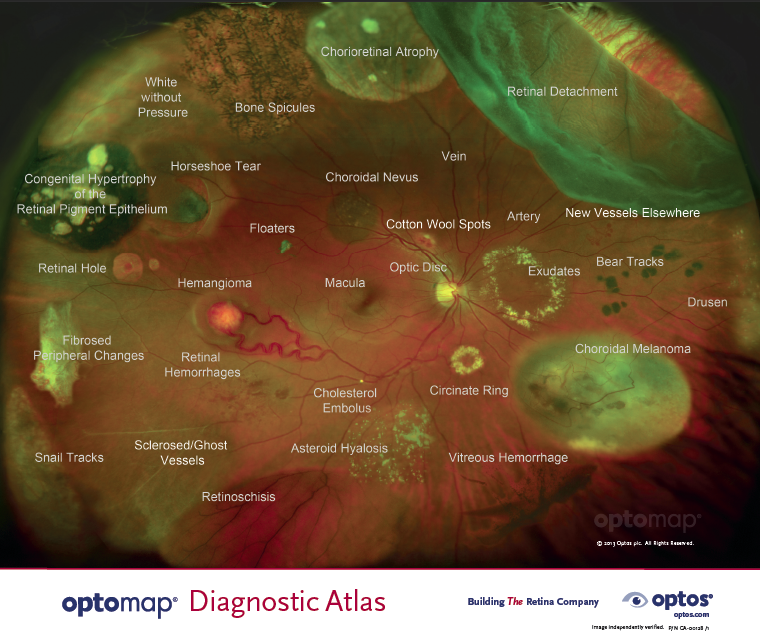
Many pathologies, including choroidal nevi and melanoma can be detected and monitored by eyecare professionals with optomap.
Choroidal nevi are typically discovered during routine dilated fundus examinations and are usually asymptomatic. However, some may be associated with central and peripheral vision loss secondary to subretinal fluid, cystoid retinal edema or, rarely, neovascularization3. Choroidal melanoma also tend to be asymptomatic, but are more likely to be symptomatic than benign nevi, presenting as decreased vision, flashes or floaters.
In their study, Cheung et al. suggest that there are phenotypical markers and environmental risk factors that predispose a person to developing choroidal melanoma. A later study4, using choroidal nevi were also present in subjects who did not conform to a particular phenotype. Gordon-Shaag et al. concluded that it was the expanded view (200°) of ultra-widefield (UWF™) technology that improved their ability to locate nevi. This was further supported by Brett et al., who concluded that the optomap was the most effective device for pinpointing choroidal nevi5.
Historically, the challenge has been to locate the small melanoma among a cluster of choroidal nevi, since some of their features overlap, including tumor size; color, which may be pigmented or non-pigmented; location; associated quiescent features, such as overlying retinal pigment epithelium (RPE) alterations and drusen; and suspicious features, including subretinal fluid (SRF) and orange pigment.
In a study with 49 patients (29 had established melanoma and 20 had established non-malignant nevi), Kernt et al.6 investigated the imaging properties of clinically diagnosed melanocytic choroidal tumors using a UWF scanning laser ophthalmoscope with two wavelengths to distinguish between benign and malignant tumors. All patients underwent clinical examination, undilated optomap imaging, standardized ultrasound (US) examination and standard retinal photography. They found that typical malignant lesions appeared dark on the red laser channel and bright on the green laser channel. These characteristics, alone, yielded a diagnostic sensitivity of 70 percent and specificity of 76 percent. When other diagnostic findings were considered — lesion size, margin touching the optic disc, and existence of SRF — results improved to 90 percent sensitivity and 82 percent specificity. The authors acknowledge that the addition of other parameters may increase diagnostic accuracy and that larger studies need to be done to validate these findings.
There is growing evidence to support the use of the optomap for routine annual ophthalmic exams for early detection of choroidal nevi. Once identified, they can be recorded and closely monitored for signs of transformation. With regular follow-up, optomap facilitates a full range of investigations to provide eyecare professionals with the relevant information to devise an effective and timely treatment plan.

Sources:
- Singh AD et al. Ophthalmology. 2005:112 (10):1784-1789 cited in Albert Cheung, Ingrid U. Scott, MD, MPH, Timothy G. Murray, MD, and Carol L. Shields, MD – Edited by Ingrid U. Scott, MD, MPH and Sharon Fekrat, MD – Distinguishing a Choroidal Nevus From a Choroidal Melanoma. 2012. EyeNet Magazine. https://www.aao.org/eyenet/article/distinguishing-choroidal-nevus-from-choroidal-mela
- Carol L. Shields, MD; Minoru Furuta, MD; Edwina L. Berman, BS; et al. Jonathan D. Zahler, MD; Daniel M. Hoberman, BS; Diep H. Dinh, BS; Arman Mashayekhi, MD; Jerry A. Shields, MD Choroidal Nevus Transformation Into Melanoma Analysis of 2514 Consecutive CasesArch Ophthalmol. 2009; 127(8):981-987. doi:10.1001/archophthalmol.2009.151
- Albert Cheung, Ingrid U. Scott, MD, MPH, Timothy G. Murray, MD, and Carol L. Shields, MD – Edited by Ingrid U. Scott, MD, MPH and Sharon Fekrat, MD – Distinguishing a Choroidal Nevus From a Choroidal Melanoma. 2012. EyeNet Magazine. https://www.aao.org/eyenet/article/distinguishing-choroidal-nevus-from-choroidal-mela
- Gordon-Shaag A , Barnard S, Millodot M, Gantz L, Chiche G, Vanessa E, Ruth W, Pinchasov R, Gosman Z, Simchi M, Koslowe K and Shneor E. Prevalence of choroidal naevi using scanning laser ophthalmoscope. Ophthalmic Physiol Opt2014; 34: 94-101. doi: 1111/opo.12092
- Paul Brett J1, Lake A2, Downes S1,3.J Vis Commun Med. Colour imaging in the monitoring and documentation of choroidal naevi. Are Optomap colour images adequate for this purpose? 2016 Jan-Jun; 39(1-2):10-7. doi: 10.1080/17453054.2016.1182476. Epub 2016 Jun 2.
- Marcus Kernt, Ulrich C Schaller, Carmen Stumpf, Michael W Ulbig, Anselm Kampik, and Aljoscha S Neubauer (2010) Choroidal pigmented lesions imaged by ultra-wide-field scanning laser ophthalmoscopy with two laser wavelengths (Optomap) Clin Ophthalmol. 2010; 4: 829–836.