Efficacy of Utilizing Ultra-widefield Retinal Imaging to Detect Peripheral Retinal Changes in Patients with Age-Related Macular Degeneration
A recent study (Friberg, Ophthalmology Retina) evaluated morphologic and angiographic changes in the peripheral retina associated with age-related macular degeneration (AMD) using ultra-widefield (UWF™) retinal imaging. The purpose was to illuminate the potential value of using UWF optomap® imaging as a potential tool for detecting peripheral changes that could flag the early warning signs and/or progression of AMD.
AMD is a common eye condition that causes damage to the macula, and is a leading cause of vision loss among people age 50 and older. In some people, AMD advances so slowly that vision loss does not occur for a long time. In others, the disease progresses faster and may lead to a loss of vision in one or both eyes. AMD by itself does not lead to complete blindness, with no ability to see. However, the loss of central vision in AMD can interfere with simple everyday activities, such as the ability to see faces, drive, read, write, or do close work, such as cooking or fixing things around the house.1
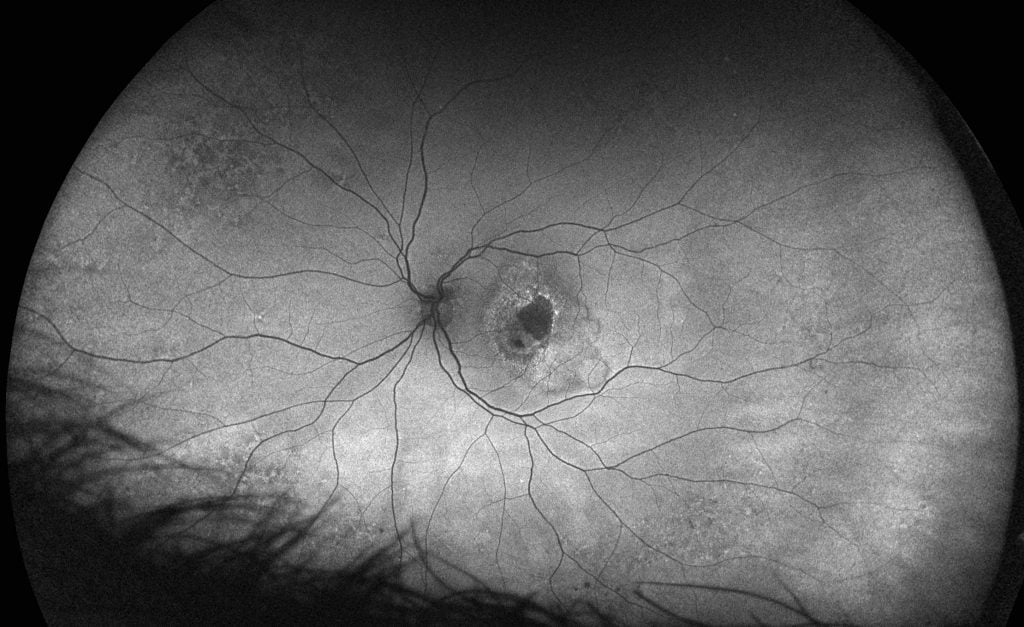
optomap af image showing Wet AMD – Courtesy of Tim Steffens
As the disease progresses through the asymptomatic phase, it moves from Dry AMD to Wet AMD. In geographic atrophy (dry AMD), there is a gradual breakdown of the light-sensitive cells in the macula that convey visual information to the brain, and of the supporting tissue beneath the macula. In neovascular AMD (wet AMD), abnormal blood vessels grow underneath the retina. These vessels can leak fluid and blood, which may lead to swelling and damage of the macula. It is important to assess the risk of progression from the dry type to the wet type of the disease.
Earlier detection and treatment of AMD can prompt steps to be taken to help reduce vision loss and slow the advance of the disease. This recent data suggests that the retinal periphery can exhibit some important morphological changes, such as peripheral drusen and reticular pigmentary changes, which are frequently connected with the wet form of AMD. Typically, disease progression has been documented using fundus cameras that image only about 45-50% percent of the retina. By using UWF for AMD evaluation, over 80% of the retina is now analyzed to record peripheral fluorescein angiographic changes in AMD patients.2
This cross-sectional study included:
- 152 patients with clinical AMD and 150 healthy controls, without AMD. Patients were 50+ years of age
- Color optomap images were captured of each group and Fluorescein angiographic images of only the AMD group.
- Morphological and angiographic peripheral retinal changes were studied per the frequency of their occurrence, the affected peripheral retina, and the localization of peripheral changes with regard to the eye equator.
The purpose of this clinical study was to compare morphological characteristics of peripheral retinal changes between AMD patients and a healthy control group, and to compare the peripheral retinal changes between the two (2) AMD types according to type, frequency, retinal periphery involvement, and localization of observed retinal changes in relation to the equator of the eye.
Color and FA images were graded by masked graders for the presence of:
- peripheral reticular pigmentary changes
- peripheral drusen
- hyperpigmented changes, such as nevi and pigmented clumping
- hypopigmented changes, such as atrophic areas or retinal pigment epithelium depigmentation.
The observed retinal changes were analyzed according to type, extent as measured in clock hours, and localization of changes with regard to the eye equator. Drusen, reticular pigmentary change, and paving stone degeneration occurred significantly more frequently in the subjects with AMD compared with the healthy eye control group and white without pressure degeneration was present in a high percentage of control subjects.
Conclusion
Retinal changes were observed peripheral to the equator in more than 40% of analyzed eyes in patients with and without AMD. And because of the increased retinal capture, it was demonstrated that 40% of drusen was detected via optomap imaging outside of the equator at 150 degrees, thereby intimating the successful efficacy of the use of UWF for detecting peripheral markers that may lead to AMD.
optomap UWF imaging is a proven tool for effective clinical decision making. More than 400 published and ongoing clinical trials, as well as thousands of case studies and testimonials, show the long-term value of optomap imaging in diagnosis, treatment planning, and patient engagement. optomap is a proven tool for effective clinical decision making. Add optomap to your practice today.
1Age-related Macular Degeneration, National Eye Institute
2Thomas R. Friberg, MS, MD, et al. Morphological and Angiographic Peripheral Retinal Changes in Patients with Age-Related Macular Degeneration. American Academy of Ophthalmology, Ophthalmology Retina Sept 2017