Ultra-widefield Imaging Characterizes Peripheral Retinal Changes Associated with AMD
Age-related macular degeneration (AMD) is the world’s third most common cause of vision impairment and the primary cause of vision impairment in industrialized nations. With age being the most important risk factor, eye care practitioners serving rapidly aging populations can expect to see a growing number of AMD patients.
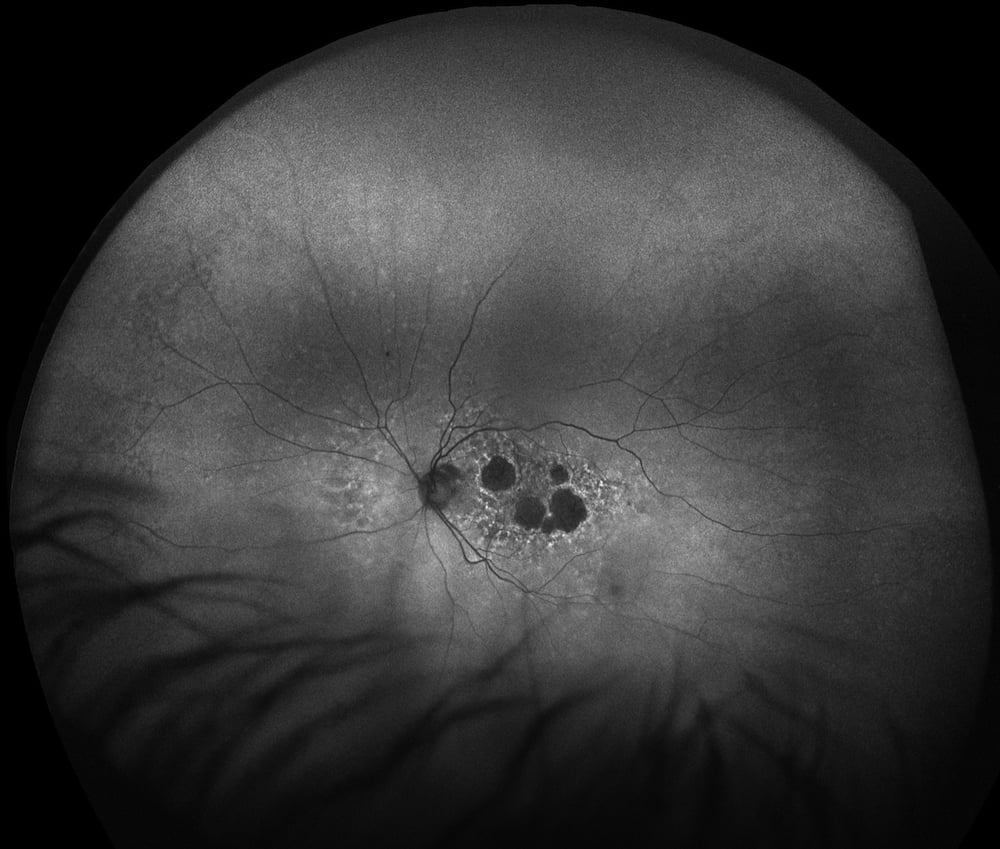
Age-related Macular Degeneration (AMD), AF
Ultra-widefield (UWF™) retinal imaging technology is now being used to characterize the peripheral vascular abnormalities associated with AMD as part of ongoing research into improved methods for diagnosis and treatment. One observational study, Peripheral Autofluorescence and Clinical Findings in Neovascular and Non-neovascular Age-related Macular Degeneration, has used both UWF fundus autofluorescence (FAF) and UWF color imaging to understand if peripheral FAF abnormality patterns are different in patients with neovascular and non-neovascular AMD.
About Ultra-Widefield Retinal Imaging
UWF retinal imaging is performed by a specially designed scanning laser ophthalmoscope (SLO) that generates a high-resolution digital image covering 200° (or about 82%) of the retina. By comparison, conventional 7 standard field (7SF) ETDRS and fundus camera photographs produce a relatively narrow view (75° or less) of the center-portion of the retina.
The SLO simultaneously scans the retina using two low-power lasers (red – 633 nm and green – 532 nm) that enable high-resolution color imaging of retinal substructures. The resulting UWF digital image – the optomap – is produced in a single capture, often without pupil dilation.
Along with UWF color imaging, the technology supports UWF fluorescein angiography (FA), UWF fundus autofluorescence (FAF), red reflectance imaging (RR), and UWF indocyanine green chorioangiography (ICG).
Study Subjects and Methods
The study examined two groups of patients, one group of 100 patients (200 eyes) with neovascular or non-neovascular AMD, and a second group of 19 (38 eyes) with no disease. Patients with AMD had a mean age of 80.3 years old compared to the normal group with a mean age of 68.8 years. There were no other significant differences (e.g. co-morbidities like diabetes) between the groups.
Subjects were examined using both UWF color and FAF imaging, and while not required, eyes were dilated. Ultra-widefield FAF uses the SLO’s green (523 nm) scanning laser to image lipofuscin autofluorescence within the retinal pigment epithelium (RPE). UWF color imaging was used to correlate FAF observations.
The study defined peripheral autofluorescence abnormalities as those outside of the centrally-located “field 2” on reference ETDRS 7-field photography. Increased or decreased autofluorescence compared to the FAF image background was evaluated as well as appearance and location around the periphery. FAF abnormalities were visually classified as granular (points of increased autofluorescence indicating drusen), mottled (areas of decreased autofluorescence signifying RPE depigmentation), or nummular (areas of decreased autofluorescence corresponding to RPE atrophy), per definitions developed in a previous study, Prevalence of Peripheral Abnormalities on Ultra-widefield Greenlight (532 nm) Autofluorescence Imaging at a Tertiary Care Center2.
Results
FAF imaging found that only 18.4% of eyes in the normal group had any peripheral abnormalities. In contrast, 72.8% of eyes with non-neovascular AMD had FAF abnormalities. For eyes with neovascular AMD, 86.0% had abnormalities. Other findings included:
— There was strong correlation between the peripheral abnormalities uncovered in the FAF images and the peripheral abnormalities observed in the color images (i.e., peripheral drusen, cobblestone degeneration, and RPE depigmentation). Over 96% of eyes with FAF abnormalities were also found to have abnormalities on the color images.
— All types of FAF abnormalities (granular, mottled, or nummular areas) were more frequent in patients with neovascular AMD as compared to those with non-neovascular AMD.
— Statistical analyses of the results suggested that the type of AMD (non-neovascular versus neovascular), rather than age, was the major reason for variations in the frequency of abnormalities.
— Almost 90% of patients had the same pattern (or patterns) of FAF abnormalities in both eyes. The authors observed that this, plus similar findings in other studies, gives weight to the hypothesis that genetic factors may be playing a role in the progression of AMD, and so could be a topic for further investigation.
— The study’s authors also noted that 77.3% of the women in the study were found to have peripheral FAF abnormalities versus 59.1% of the men. This was also noted as an area for additional research.
With FAF an established diagnostic technique for the early detection and management of AMD, UWF FAF is giving researchers and practitioners a more comprehensive understanding of how the disease progresses. Future studies may provide additional insight into the possible prognostic value of early characterization of peripheral FAF abnormalities.
Sources:
- Tan, Colin S. et al., Peripheral Autofluorescence and Clinical Findings in Neovascular and Non-neovascular Age-related Macular Degeneration, Ophthalmology , Volume 120 , Issue 6 , 1271 – 1277
- Heussen FM, Tan CS, Sadda SR. Prevalence of peripheral abnormalities on ultra-widefield greenlight (532 nm) autofluorescence imaging at a tertiary care center. Invest Ophthalmol Vis Sci 2012;53:6526 –31.