A common complication arising from diabetic vitrectomy for the treatment of proliferative diabetic retinopathy (DR) is recurrent post vitrectomy diabetic vitreous hemorrhage (PVDVH). A recent study1 using ultra-widefield fluorescein angiography (UWF FA) has generated new insights into the etiology of recurrent PVDVH. The study results also suggest that imaging of the peripheral retina may provide practitioners with superior, actionable post-operative information compared to conventional imaging techniques.
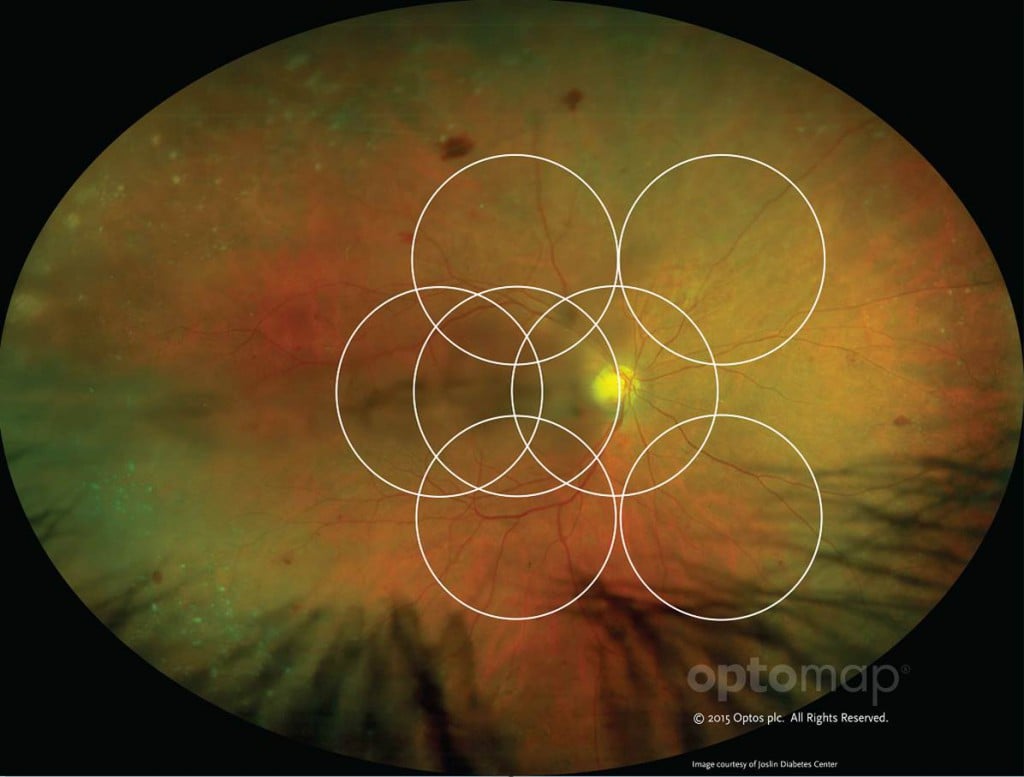
optomap image as compared to ETDRS 7 standard fields.
Multimodal UWF Retinal Imaging
UWF retinal imaging is performed using a specially-designed scanning laser ophthalmoscope (SLO) that generates a high-resolution digital image – optomap – which captures 200° (or about 82%) of the retina. By contrast, conventional ETDRS 7 standard field (7SF) photographs produce a relatively narrow view (45° or less) of the center-portion of the retina.
For UWF color imaging, the SLO simultaneously scans the retina with two low-power lasers (red and green) that enable high resolution, color imaging of retinal substructures. The scan is completed in a single capture in less than a second, often without pupil dilation required. Along with UWF color imaging, the technology also supports ultra-widefield fluorescein angiography (FA), UWF fundus autofluorescence (FAF), and UWF indocyanine green chorioangiography (ICG).
PVDVH Study Background
The study examined a group of patients who had recurrent PVDVH after undergoing three-port pars plana vitrectomy for diabetic vitreous hemorrhage or tractional retinal detachment. The study group received panretinal photocoagulation (PRP) treatment before or during the vitrectomy, and had at least one intravitreal bevacizumab injection over the course of PVDVH treatment. UWF FA imaging was undertaken more than one month after each patient’s last bevacizumab injection.
The study also examined a control group consisting of patients without recurrent vitreous hemorrhage after the same three-port pars plana vitrectomy for diabetic vitreous hemorrhage or tractional retinal detachment.
The study’s primary objective was to identify differences in UWF FA findings between patients with and without recurrent PVDVH. A secondary objective was to compare UWF FA findings with conventional 7 standard fields angiography.
Key Results and Discussion
The study was conducted on 22 eyes with PVDVH and 24 eyes without. Despite the smaller sample size, UWF FA imaging revealed statistically significant differences in pathological findings in the retinal periphery between patients with and without recurrent PVDVH:
— Eyes with PVDVH showed higher instances of peripheral neovascularization (40.9% vs. 8.3%; P = 0.010)
— Eyes with PVDVH showed higher instances of peripheral nonperfusion (81.8% vs. 37.5%; P = 0.002)
— Eyes with PVDVH showed higher instances of late peripheral vascular leakage (90.9% vs. 29.25%; P < 0.001)
What makes these results more striking is that when patient UWF FA images were cropped down to the size of conventional 7SF and independently evaluated, there were no statistically significant differences in rates of peripheral neovascularization, nonperfusion or vascular leakage between eyes with and without PVDVH.
While not directly examined in the study, the authors suggested that increased, post-operative levels of vascular endothelial growth factor (VEGF) could:
— Promote peripheral retinal neovascularization or fibrovascular proliferation at the sclerotomy site, which in turn could contribute to subsequent PVDVH.
— Promote higher rates of peripheral nonperfusion and late peripheral vascular leakage which, based on their work, appears to be closely associated with PVDVH.
With increased VEGF expression as a potential causative factor for PVDVH, the study’s authors hypothesized that additional, post-operative panretinal photocoagulation (which can reduce vitreous fluid VEGF concentrations) or intravitreal bevacizumab maintenance treatments could improve PVDVH outcomes for patients with peripheral neovascularization, nonperfusion or vascular leakage. In fact, during the study patients with PVDVH who received PRP or intravitreal bevacizumab maintenance treatments had few recurrences – 10% of those receiving PRP and 16% of those receiving injections. While these results were not statistically significant, they are not consistent with the suggested link between higher post-operative levels of VEGF and PVDVH.
The other major takeaway of the study is the role UWF retinal imaging can play in diabetic vitrectomy post-operative care. The study found that the use of conventional 7SF in post-operative evaluation can miss important associated pathologies. Especially in patients with recurrent PVDVH, UWF visualization of the retinal periphery can give practitioners a deeper understanding of individual patient progress and provide guidance about the potential efficacy of PRP, intravitreal bevacizumab, or other treatments to relieve PVDVH and restore patient vision.

[1] Kim DY, Kim J-G, Kim YJ, et al. Ultra-widefield fluorescein angiographic findings in patients with recurrent vitreous hemorrhage after diabetic vitrectomy. Invest Ophthalmol Vis Sci. 2014;55:7040-7046.