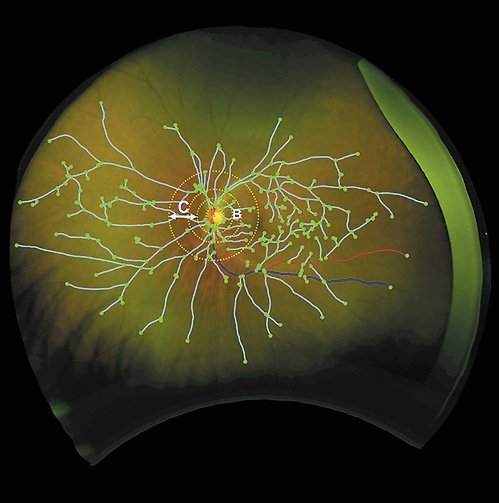
In a novel study from Queen’s University Belfast, researchers demonstrate that the eye could be a window to the brain. The results of the study, recently published in the Journal of Ophthalmic Research, show how degenerative brain diseases such as Alzheimer’s Disease (AD) can be monitored via ultra-widefield (UWF) retinal imaging. The retina is a part of the central nervous system and shares structural and functional features with the brain. Altogether 59 AD patients and 48 controls were entered into the study. They were imaged utilizing ultra-widefield imaging from Optos. This advanced technology, using red and green lasers, captures a 200 degree, high-resolution digital image of the retina in less than ½ second, reaching regions of the retina that have been previously inaccessible with other methods of imaging.
Measuring biomarkers, such as drusen and vasculature width gradients in delineated quadrants of the retina, the researchers found that these changes, particularly in the peripheral retina, could be associated with degenerative brain conditions such as AD. Specifically, the markers that were chiefly considered were drusen and vasculature changes. Drusen are deposits of fats, minerals, and proteins and are normal symptoms of aging that appear as yellowish spots in the layer beneath the retina. While they are harmless and typically begin to appear after the age of 40, an increased occurrence in number and size can contribute to the degeneration of the retina. In the study, at baseline and follow up, the optomap images revealed that drusen accumulation, particularly in the superior nasal quadrant, were increased and significantly associated with positive AD status as compared to the number of drusen that would be normally expected in the control group. An additional novel element of the study was that by utilizing the UWF view of optomap, the width gradient of the vasculature could be observed in entirety from the macula to the far retinal periphery. The study found that people with AD have blood vessels that are wider closer to the macula and thin as they progress further into the periphery. This can impede the flow of blood and the essential delivery of nutrients and oxygen in the periphery, leading to further damage.
The team, led by Dr. Imre Lengyel of Queen’s University, hypothesized that changes in the peripheral retina could be important to explore the association between the eye and the brain. They concluded that their research supported their original hypothesis and that UWF retinal imaging has significant potential for monitoring AD and other degenerative brain diseases via the eye. Utilizing optomap to evaluate progression of AD may bring important value to this effort because changes in the eye are easier to measure in relation to other methods necessary to evaluate the health of the brain. Establishing an evidential correlation between the eye and the brain would suggest that utilizing UWF imaging could provide an easier, more expedient access to that information. Furthermore, UWF imaging provides a much less expensive option to other methods of evaluation, such as brain scans. The researchers demonstrated that by utilizing optomap, they were able to identify early markers that could manifest many years before dementia develops as well as high risk groups who would benefit from preventative guidance. The study notes that to be a reasonable marker of early disease, pre-symptomatic, or early symptomatic patients would need to be followed up over several years to determine the predictive value of the peripheral findings. Routine optomap exams could prove to be an earlier, easier and more cost-effective method for monitoring the progression of AD, and identifying individuals at high-risk of developing AD.
Read the Full Article here….
Or visit our website to learn more about clinical studies utilizing optomap technology.