Age-related macular degeneration (AMD) is one of the leading causes of blindness in adults over age 50 and it affects about 2.1 million people in the US. Early diagnosis and treatment are the keys to preventing vision loss. AMD is a degenerative disease that happens when part of the retina called the macula, is damaged. The macula is the part of the eye that delivers sharp, central vision needed to see objects straight ahead. Over time, the loss of central vision can interfere with everyday activities, such as the ability to drive, read, and see faces clearly.
During AMD Awareness Month in February, the American Academy of Ophthalmology is reminding people that even though there is not currently a cure for AMD, there are a number of things you can do to slow its effects and prevent blindness, early detection being a critical first step. Treatments for macular degeneration depend on whether the disease is in its early-stage, dry form or in the more advanced, wet form that can lead to serious vision loss.
What is AMD?
– AMD is a common eye condition and a leading cause of blindness in those 50 and older. Aging can cause the macula to slowly degenerate and reduce central vision.
– AMD often advances so slowly that vision loss does not occur for many years and traces of the disease can go unnoticed. In others, the disease may progress faster and lead to vision loss in one or both eyes. Over time, objects in vision may not appear as bright as they once were and a blurred area in vision is common, further leading to blank spots in vision.
-AMD ultimately results in a loss of central vision that can interfere with simple everyday activities.
Dry Vs Wet AMD
Wet AMD occurs when abnormal blood vessels behind the retina start to grow under the macula. These new blood vessels tend to be very fragile and often leak blood and fluid. The blood and fluid raise the macula from its normal place at the back of the eye. Damage to the macula occurs rapidly. With wet AMD, loss of central vision can occur quickly. Wet AMD is considered to be advanced AMD and is more severe than the dry form.
Dry AMD occurs when the light-sensitive cells in the macula slowly break down, gradually blurring central vision in the affected eye. As dry AMD gets worse, you may see a blurred spot in the center of your vision. Over time, as less of the macula functions, central vision in the affected eye can be lost gradually.
The most common symptom of dry AMD is slightly blurred vision. You may have difficulty recognizing faces and may need more light for reading and other tasks. Dry AMD generally affects both eyes, but vision can be lost in one eye while the other eye seems unaffected.
One of the most common early signs of dry AMD is drusen. Drusen are yellow deposits under the retina. They often are found in people over age 60. Your eye care professional can detect drusen during a comprehensive eye exam.
Steps to Take Control of Your Eye Health
Regular comprehensive eye exams. AMD often has no symptoms prior to onset, so getting regular exams is critical to diagnosing and treating eye disease in its early stages.
Quit smoking. Numerous studies show smoking increases the risk of developing AMD, and the speed at which it progresses. Smokers are twice as likely to develop macular degeneration compared with a nonsmoker.
Eat a well-balanced diet. Eating a diet rich in fruits, vegetables, and nutrient-packed foods, such as salmon and nuts, may reduce the risk of AMD.
Take the right kind of vitamins. Vitamins may delay the progression of advanced AMD and help people keep their vision longer if they have intermediate AMD or advanced AMD in one eye.
Exercise regularly. Exercising three times a week can reduce the risk of developing wet AMD by 70 percent. Studies also show that physical activity may lower the odds of both early and late-stage AMD.
Monitor your sight with an Amsler Grid. This simple routine takes less than one minute and can help people with AMD save more of their vision. Using this grid is essential to finding any vision changes that are not obvious, so you can report them to your eye care professional.
AMD Detection
AMD is usually detected during a comprehensive eye exam. During an eye exam, you may be asked to look at an Amsler grid. The pattern of the grid resembles a checkerboard. You will cover one eye and stare at a black dot in the center of the grid. While staring at the dot, you may notice that the straight lines in the pattern appear wavy. You may notice that some of the lines are missing. These may be signs of AMD.
If your eye care professional believes you need treatment for wet AMD, he or she may suggest a fluorescein angiogram. In this test, a special dye is injected, and pictures are taken as the dye passes through the blood vessels in your retina. The test allows your eye care professional to identify any leaking blood vessels and recommend treatment.
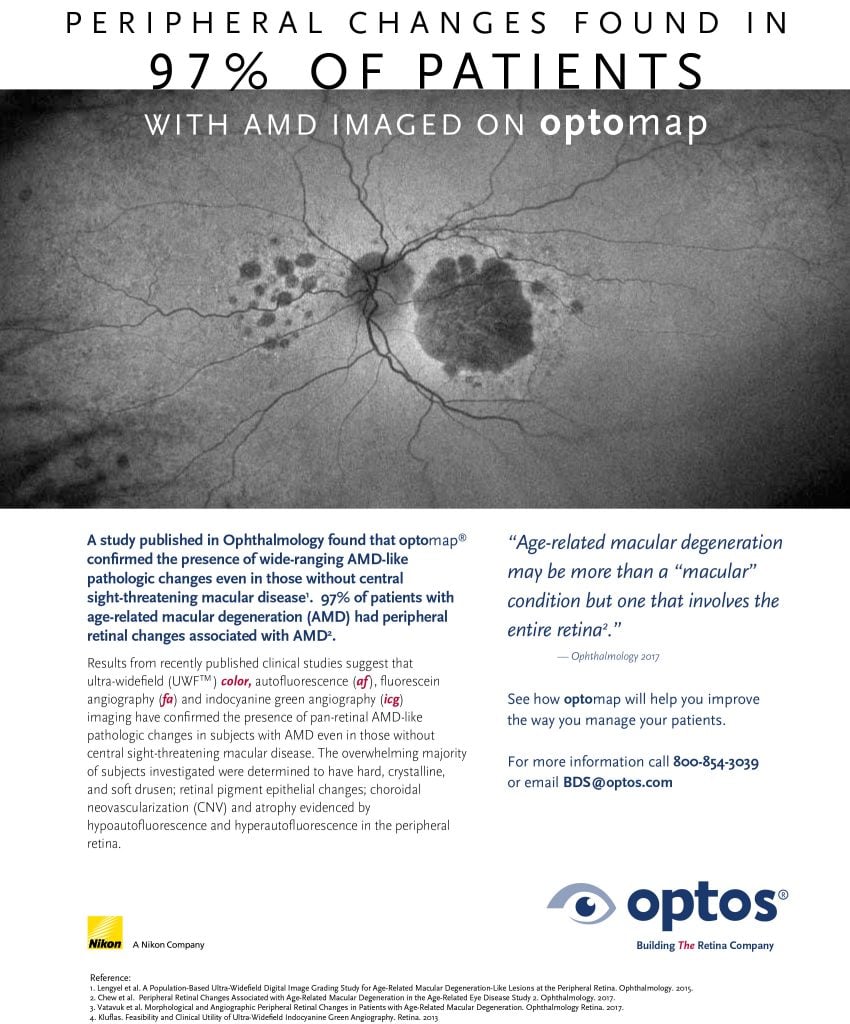
Peripheral Retinal Changes Associated with Age-Related Macular Degeneration
The 12-year follow-up of a study known as the Reykjavik Eye Study evaluated subjects with optomap color and autofluorescence imaging and found that 67% of subjects in the study had peripheral AMD-like changes. Additionally, a subsequent study, knowns as the OPERA (Optos Peripheral RetinA) study found that peripheral retinal changes were more prevalent in eyes with AMD than in those without. Drusen were evident in the majority of the eye with AMD in both the mid and far periphery. These studies go to show that AMD may be more than a “macular” condition but one that involves the entire retina. Other research also shows that optomap UWF icg captured significant peripheral changes in 80% of AMD patients. These studies all contribute to the benefits of ultra-widefield imaging in the diagnosis and management of AMD. Future longitudinal studies of peripheral changes in AMD and their impact on visual function may also contribute to further understanding of the disease. Click here for more information regarding these studies or visit our website to learn more about optomap and how it helps eyecare professionals to manage eye disease.